CMS’ GUIDE Model

Centers for Medicare & Medicaid Services’ Guiding an Improved Dementia Experience (GUIDE) Model: Care Affordability and the Burden on Unpaid Caregivers for Beneficiaries with Dementia
About 6.7 million Americans age 65 or older currently live with Alzheimer’s disease or another form of dementia, with projections putting that number closer to 14 million by 2060. Estimates show that the total healthcare costs for this population will reach $345 billion in 2023, with Medicare and/or Medicaid covering 64% of that cost. However, patients and their family still face a significant financial burden – on average, Medicare beneficiaries with Alzheimer’s or other dementias face an annual out-of-pocket cost of $10,241, compared to $2,518 for those not suffering with these diseases.
Affordability may prevent patients from seeking care in a timely manner. Using 2020 Medicare Current Beneficiary Survey data, it’s estimated about 6.4% of Medicare beneficiaries age 65 and older with Alzheimer’s or other dementias reported delayed care due to cost, compared to 5.4% of those without.
In addition, many people with Alzheimer’s or other dementias live with and depend on family and friends to help with their care; more than 80% of the care provided to this population is estimated to come from family, friends or other unpaid caregivers. Considering these factors makes the financial and emotional toll for dementia care even more acute.
Guiding an Improved Dementia Experience (GUIDE) Model
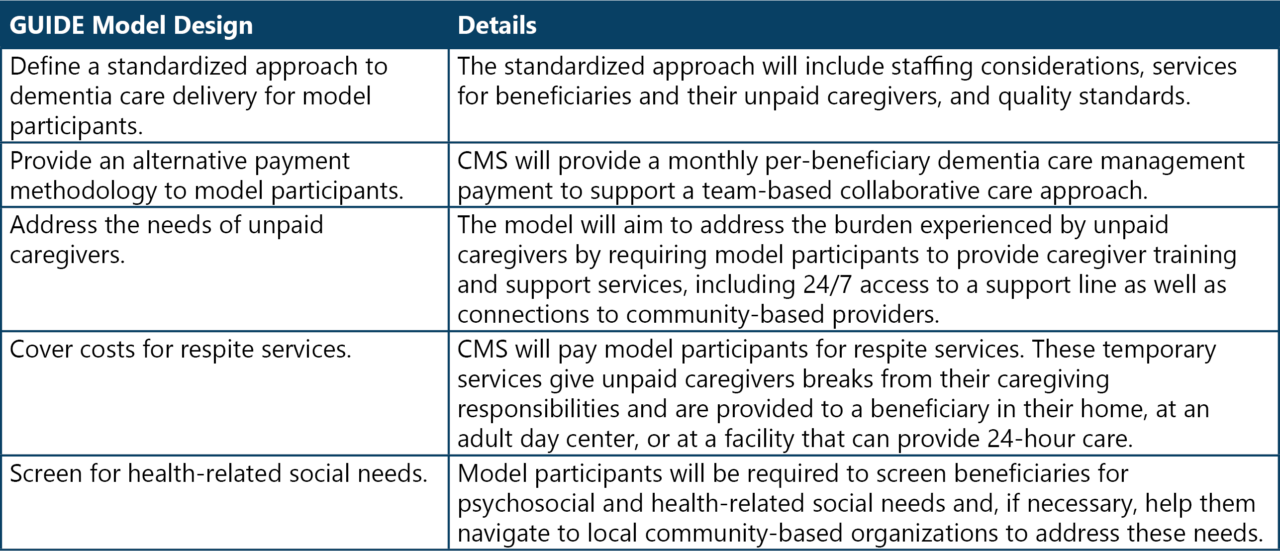
To improve the quality of care for people living with Alzheimer’s or other dementias and reduce the strain on their unpaid caregivers, the Centers for Medicare & Medicaid Services (CMS) announced the GUIDE Model on July 31, 2023. This eight-year, nationwide voluntary model launches on July 1, 2024. It is designed to attract a range of Medicare Part-B enrolled providers and practitioners to establish dementia care programs that provide ongoing, longitudinal care and support to people living with dementia through an interdisciplinary team . The GUIDE Model aims to address the key drivers of poor-quality dementia care in five ways (Table 1):
Table 1: The GUIDE Model
Impact of the GUIDE Model
The GUIDE Model can effectively address beneficiaries’ affordability by offering a new payment to participants for respite services furnished to aligned beneficiaries and their caregivers. Additionally, the requirement for model participants to screen beneficiaries for health-related social needs and help navigate them to community-based sources of care also aids in addressing affordability. Ultimately, a primary goal of the model is delaying long-term nursing home care, which is the biggest source of out-of-pocket costs for people living with dementia.
The GUIDE Model can also reduce the burden and strain on unpaid caregivers of beneficiaries living with dementia by providing caregiver training, referrals to community-based social services and supports, 24/7access to a support line, and temporary respite services. In addition, a caregiver burden measure will be developed in the first year of the GUIDE Model to be part of the model’s five performance metrics for dementia care management payment adjustment calculations.
As a contractor who has supported CMS on numerous initiatives, RELI Group applauds CMS’ efforts to improve the quality of dementia care and tackle the obstacles facing beneficiaries and their caregivers through the GUIDE model. Look for our follow-up post when data on this project is released – in the meantime, feel free to check out our other articles and blogs!














